In this study, researchers investigated the potential benefits of combining dendritic cell (DC) with autologous cytokine-induced killer (CIK) immunotherapy alongside high-dose chemotherapy (HDC) for patients with metastatic breast cancer (MBC). The results of the study showed that the HDC and DC/CIK combination therapy was highly effective for MBC patients. Specifically, the use of a specific HDC regimen in conjunction with DC/CIK immunotherapy showed promising clinical benefits when compared to chemotherapy alone. This research highlights the potential of combining different treatments to provide patients with a more comprehensive and effective approach to cancer treatment.
Selections of appropriate regimen of high-dose chemotherapy combined with adoptive cellular therapy with dendritic and cytokine-induced killer cells improved progression-free and overall survival in patients with metastatic breast cancer: reargument of such contentious therapeutic preferences.
Selections of appropriate regimen of high-dose chemotherapy combined with adoptive cellular therapy with dendritic and cytokine-induced killer cells improved progression-free and overall survival in patients with
metastatic breast cancer: reargument of such contentious therapeutic preferences.
Our previous work showed thiotepa could eradicate breast cancer stem cells. From 2004 to 2009, 79 patients received standard dose chemotherapy (SDC) of 75 mg/m2 docetaxel and 75 mg/m2 thiotepa versus 87 patients of HDC – DC/CIK: 120 mg/m2 docetaxel to mobilize peripheral CD34? progenitor cells, a sequence of HDC (120 mg/m2 docetaxel, plus 175 mg/m2 thiotepa) – DC/CIK, with or
without 400 mg/m2 carboplatin depending upon bone marrow function.
The endpoints were response rates (RR), progression-free survival (PFS), and overall survival (OS).
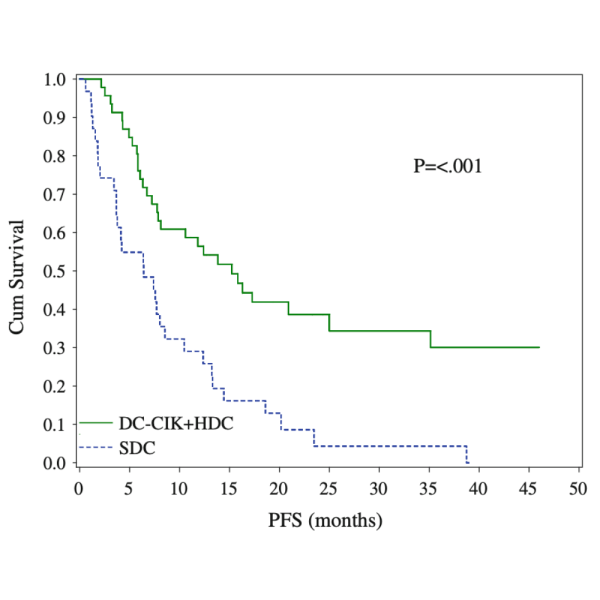
Results Compared with SDC, PFS and OS were improved in HDC – DC/CIK (median PFS 10.2 vs. 3.7 months,P \ 0.001; median OS 33.1 vs. 15.2 months, P \ 0.001). Patients of pre-menopausal, HDC as first-line treatment after metastasis, or with visceral metastasis showed pro- longed PFS and OS. SDC group also achieved the similar response as previous reports.
Although this study could not be regarded as an entire prospective clinical trial, 166 patients in this comparative study were divided into HDC plus adoptive cellular therapy with DC/CIK cells or standard dose chemotherapy. While the complex nature of our treatment regimen will require additional studies to determine the role of each of the components, including autologous DC, CIK, and high-dose docetaxel and thiotepa, we have demonstrated the feasibility and tolerability of a thera- peutic regimen combining chemo plus immunotherapy. To our knowledge, it might be the first trial to combine all of the elements in the treatment of patients
with MBC.
This study demonstrated the novel combina- tion of HDC with DC/CIK to be an effective choice for the selected MBC population, in which choosing appropriate chemo regimens played important roles, and also specific HDC regimen plus DC/CIK immunotherapy showed the clinical benefits compared with chemotherapy alone.
Article Reference link: click here
Scientific article publishing date 3/1/2013
REGISTERED ADDRESS:
Immunyo Ltd
Kincora Ave 35
Clontarf
Dublin 3
Ireland
For Germany, Austria and Switzerland